Do I Have Hip Bursitis … Probably Not | Hip Bursitis Treatment Toronto
My doctor said it’s hip bursitis. It can be very frustrating to see a patient who has been misdiagnosed and suffered with a condition that has prevented them from doing the activities that they love to do. On the flip side, it is so rewarding to provide them with the proper diagnosis and treatment plan, to help alleviate an issue that should have been relatively easy to manage.
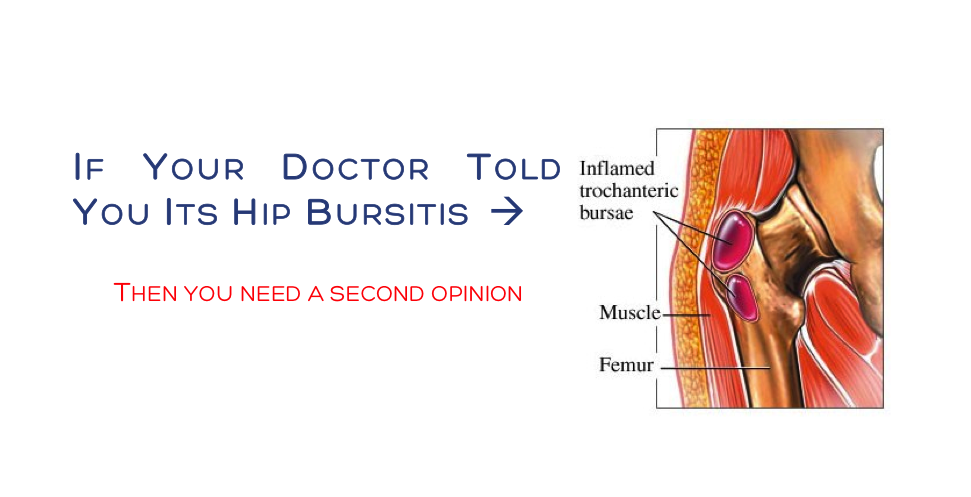
To get the best results, there are times when knowing the etiology and physiology of a particular condition is really important (more than usual). It is going to change how treatment is approached based on what certain conditions respond best to. This is especially true of greater trochanteric pain syndrome (GTPS), which is colloquial known as trochanteric bursitis. It is one of the most common causes of hip pain (2nd), and is a frequent reason for a visit to one’s medical doctor for those over 35 (especially females).
You might have GTPS if you have…
Chronic, or acute intermittent pain, or tenderness over the lateral aspect of the hip. Pain over of near the outside of the femur.
Aggravating factors include prolonged single-leg stance, lying on the affected hip, standing or transitioning to a standing position, sitting with the affected leg crossed, climbing stairs, running or other high impact activities
You Probably Dont Have Bursitis 
Today thousands of medical doctors (and unfortunately some chiros and physios) in the United States and Canada are going to diagnose and tell their patients they have bursitis of the hip. They will tell them to go home and rest, take medication. If that does not work then they may prescribe an injection of anesthetic or corticosteroid. The problem is that in most cases, people are likely being misdiagnosed with a hip bursitis when in fact they a muscle problem.
Research has shown that most people do not have bursitis of the hip in these cases of lateral hip pain. Rather they have degenerative tendinopathies or tears of the gluteus medius and or gluteus minimus. If bursitis is actually present (<20% of cases) , it is possible that it might be the result of the existing gluteus medius / minimus tendon pathology.
It is not a mistake where misdiagnosis is going to kill anyone but knowing that the two conditions will respond to different types of treatment might prevent someone from getting back to being active and doing what they love sooner. We all want to feel and move better right!
As with tendinopathies of the ankle, shoulder, or elbow, they do not respond entirely well to rest, medication or injections. Rather, tendinopathies require loading of the damaged muscle and tendon complex to promote healing and regeneration and restore strength. Eccentric and strengthening exercises are important to both strength and heal a damaged tendon and reduce this conditions reoccurrence.
These conditions also require that manual therapy, acupuncture and ergonomic suggestions are used to restore movement balance and correct for altered biomechanics (limb length inequality, obesity, hip/core weakness, altered foot mechanics, ITB tightness etc) that might have led to the exacerbation of the condition in the cases.
Rest and medication are going to do little to promote healing in a damaged tendon and alter the biomechanics of the body and cause of GTPS. For these reasons, those treated with rest, pharmaceuticals alone and / or corticosteroid, have a high recurrence rate. It is interesting to note that corticosteroid injections performed with advanced imaging guidance (ultrasound usually), do not produce superior results than those done without. Odds are that injections accidentally placed into the extrabursal space when performed without imaging guidance, are having results because they are affecting the injured tendons.
Getting the diagnoses right is important and knowing the recent state of the literature helps you get there. As with any health concern, always look for a second opinion if you are not happy with the first. In addition to this, do your own research and make sure that you are getting the treatment that is right for you. If your doctor tells you have hip bursitis, it might be time for that second opinion
References
Del Buono, Angelo, et al. “Management of the greater trochanteric pain syndrome: a systematic review.” British medical bulletin 102.1 (2012): 115.
Michaud, Thomas C. Human locomotion: the conservative management of gait-related disorders. Newton Biomechanics, 2011.
Rompe, Jan D., Neil A. Segal, Angelo Cacchio, John P. Furia, Antonio Morral, and Nicola Maffulli. “Home training, local corticosteroid injection, or radial shock wave therapy for greater trochanter pain syndrome.” The American Journal of Sports Medicine 37, no. 10 (2009): 1981-1990
Ruta, Santiago, et al. “Ultrasound evaluation of the greater trochanter pain syndrome: bursitis or tendinopathy?.” JCR: Journal of Clinical Rheumatology21.2 (2015): 99-101.
Williams, Bryan S., and Steven P. Cohen. “Greater trochanteric pain syndrome: a review of anatomy, diagnosis and treatment.” Anesthesia & Analgesia 108.5 (2009): 1662-1670.
Woodley, Stephanie J., Helen D. Nicholson, Vicki Livingstone, Terence C. Doyle, Grant R. Meikle, Janet E. Macintosh, and Susan R. Mercer. “Lateral hip pain: findings from magnetic resonance imaging and clinical examination.” The Journal of orthopaedic and sports physical therapy 38, no. 6 (2008): 313-328