Knee Pain Relief Toronto | Relief for Patellofemoral Pain Syndrome in Toronto
… I rarely see knee pain that is actually a knee problem!
If you have recurrent frontal knee pain with activity or sitting, especially if there wasn’t an accident or “ouch” moment that started it, there is something really important you need to know…

YOU PROBABLY DO NOT HAVE A KNEE PROBLEM! AND RELIEF FOR PATELLOFEMORAL PAIN SYNDROME IN TORONTO COMES FROM FIXING THE SPINE, HIPS AND FEET!
That’s right. Unless you damaged something in your knee through trauma, the odds are that your knee pain is being caused by a hip, spine and/or potentially a foot problem.
If YouTube or your manual therapist only has you doing stretching/strengthening exercises for your knee and thigh then you are likely not getting to the root of the problem.
Finding knee pain relief in Toronto from your doctor or therapist should include a comprehensive assessment to find the root cause. If your doctor or physio or traditional chiropractor is only “treating” your knee and has not assessed your spine, hips or foot then you should be asking them “why not” and “how do you know that the underlying cause is not from the hip?”.
Our Approach To Knee Pain Relief in Toronto Is Different
At our office in Yorkville Toronto, we have seen and helped hundreds of cases of atraumatic knee pain! Rarely is there a case that we can’t help with, as long as there isn’t an underlying structural problem requiring surgery or traditional medical care.
The key to our high success rate is that we always look for the underlying problem(s) that cause the health issues our patients seek us out for and not merely focus on the symptoms. You’ll get the most relief from patellofemoral joint pain or just about any health issue by addressing the Core Problem.
Whether it is the knee, spine, headaches or dozens of other health conditions we help with, finding and correcting the underlying problem(s) is the key to better health and long-term success!
[You can read more about OUR PROCESS here]
Most Pain Around The Knee Cap (without trauma) Is Patellofemoral Pain Syndrome | Patellofemoral Joint Pain Treatment in Toronto
Patellofemoral Pain Syndrome (PFPS) is the retropatellar (behind the patella/knee cap) and peripatellar (around the knee cap pain) pain that almost everyone has experienced at some point in their lives.
It is associated with lower limb loading activities such as walking, running, jumping, stair climbing and prolonged sitting and kneeling when the nerves/tissues around or behind the kneecap get irritated from repetitive strain and send a pain signal to your brain.
PFPS is the most common overuse injury of the lower extremity so if you have not experienced it consider yourself lucky!
In most cases, such as with a misstep, riding a poorly fitted bike or prolonged periods of sitting, the irritation and subsequent pain are temporary and thankfully fleeting.
This post, however, is for those for whom the pain lingers OR who want to act preventatively to keep their knees healthy for the rest of their lives!
Keep in mind that all pain does NOT represent damage to a body part. Pain is simply your body’s way of telling you that something is irritated or could become irritated if the repetitive strain continues in the same way. We are experts at helping patients fix the underlying problem and find long lasting knee pain relief in Toronto because we understand this.
In most cases, especially with PFPS, that pain is a “check engine light” trying to alert you that your knee is not moving properly and that it is being strained repetitively and COULD end up becoming injured or damaged. If your knee pain persists and it is painful to move or sit for long periods then it is likely that the knee cap and knee joint tissues have become repetitively strained, irritated and the nerves in the area of relaying a warning signal to your brain in the form of pain that something is or could become seriously wrong!
What Is Patellofemoral Pain Syndrome
If you have knee pain that began without trauma and is localized around the knee cap (patella) or underneath it, you could have PFPS.
It is typically dull, achy and/or can be sharp with weight-bearing activities or fast movements. It is typically aggravated by extended periods of sitting/positions when the knee is bent for an extended period of time or weight-bearing activity; most often stair use, walking and running. This is the type of knee pain that most cyclists feel when they have a poorly fitted bike.
Females are at greater risk of PFPS although males do experience the complaint. Males have been shown to have different mechanics from females during functional activities like running, cutting, squatting and landing. Having wider hips (on average) and a more severe angle between the thigh and knee is thought to put females at greater risk for this complaint. It is not known whether males with PFPS behave more like females mechanically or whether they present totally differently.
How to Diagnose PFPS / How Do I Know If I Have PFPS?
Upon examination, it will be unlikely for you or an unskilled practitioner to recreate the chief complaint making it difficult for some to diagnose. We have learned from seeing hundreds of these cases that patients with PFPS usually demonstrate increased joint line and tissue sensitivity compared to the non-painful side.
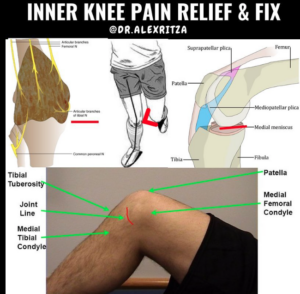
Palpation between the tibia and femur, usually the inside of the knee more than outside, will create more symptoms when the knee is examined in a 90-degree flexed position.
In chronic cases (>2-3 months), increased sensitivity in this joint line or the peripatellar joint space is a clear indication of increased local (at the knee) and/or central (spinal cord /brain) nerve sensitivity that indicates chronic neurological changes and shifts in the origin of the pain. The pain is likely being caused less by active inflammation (think swelling, heat, redness) and more by a neurological problem; increased sensitivity of the nervous system to non-dangerous stimuli like walking and climbing stairs.
Many structures have been implicated in the patellofemoral joint as pain-producing structures: subchondral bone, infrapatellar fat pad, quadriceps tendon, patellar ligament, synovium, medial and lateral retinaculum and medial and lateral patellar ligaments. There is no consensus and it frankly doesn’t matter! The pain is not the problem but more about that later!
The typical mechanism of injury is the repetitive compression of tissues under and/or around the knee cap when the knee cap moves down and deeper into the knee joint with weight bearing or prolonged flexion. Studies have shown that patellofemoral joint stress is significantly higher in patients with PFPS than those without it.
A lot of practitioners propagate the older notion that the inner quadriceps muscle (VMO) is the cause of this condition. However, the research and our experience do not support this. Altered VMO function has been implicated in a number of PFPS studies but this is not consistent across the board and it is more consistently believed that femur motion may contribute to altered knee kinematics as opposed to the abnormal patellar motion. In other words, the knee cap is not “tracking” properly in the joint because of the spine and hip biomechanics altering the movement of the thigh, which in turn affects the knee!
We will dive deeper into the role of the spine, hip and foot in PFPS below but this should make logical sense! The movement of the knee cap should be affected much less by a relatively tiny muscle on the side of the knee as opposed to the dozens or hundreds of pounds of force travelling through and altering the movement of the knee via the femur.
Why does Patellofemoral pain syndrome happen
The aetiology of patellofemoral pain syndrome is multifactorial and scientific research has indicated that there is a relationship between PFPS and:
- patellar alignment and mechanics
- foot mechanics
- hip strength and mechanics
Notice how it doesn’t say anything about a knee injury or damage!
In every case of knee pain that we come across, we always ensure that the spine, knee and ankle health is restored and magically, without touching the knee, it gets better!
Here is why the research backs this up:
Distal Factors (Foot)
Weakness, instability or a foot shape that leads to
- the mechanism of action of orthotics that helps to produce clinically significant improvements for PFPS patients is currently unclear
- it has been reported that some individuals with PFPS stand in a static stance with an externally rotated foot – read: more inward rotated tibia and more valgus force on the knee (collapse force)
- while not consistent across all studies, individuals with PFPS have been reported to have delayed/prolonged rear foot eversion during walking and running
- PFPS sufferers also reported landing with more rear foot eversion in walking and running
- Excessive rearfoot eversion with walking and running increases knee flexion and abduction which increases PFJ force
- individuals with PFPS possess increased mid-foot mobility when moving from non-weight bearing to a static relaxed stance – read: more collapse of the ankle causes more inward stress on the knee
Proximal Factors (HIP)
- individuals with PFPS have altered front and transverse plane kinematics; these changes are more likely during demanding tasks such as single-limb squat, single-limb jumping, running and lunging – read: knee collapse inward
- patellofemoral joint stress and lateral patellar tracking are increased by excessive femoral internal rotation from cadaveric and MRI studies – read: the collapse of the knee inward because of poor hip control muscle control or the femur irritates the knee
- females have greater hip abduction and external rotation than males with symptomatic females showing even greater weakness than healthy females – symptomatic females showing even greater hip adduction compared to healthy females – read: females with poor femur control from weaker glutes increases the risk of PFPS
- evidence to show that runners that go on to develop PFPS have increased hip adduction and internal rotation – read: the same point as above! The collapse of the knee inward increases the chance of developing PFPS
- some prospective evidence shows PFPS patients have delayed gluteus medius activation compared to the vasti muscles during stair-stepping tasks – read: mentioned this already – poor gluteal control and activation plays a role in PFPS

What all this data says in simple terms is this:
Inward collapse (valgus force at the knee joint, internal femoral and/or tibial rotation from the hip/foot respectively) of the knee causes poor tracking of the knee cap in its groove. This results in a repetitive strain of the knee joint tissues and the resultant inflammation, neurological change and resultant pain. Rather than the patella moving properly its groove, it is metaphorically banging into the walls of the joint over, over, and over again and this irritates the joint.
Over time, if this irritation continues it will cause increased sensitivity of the sensory nerves that signal pain to the brain from the knee, making the knee more sensitive to pain from regular activities. This is a terrible problem for chronic pain sufferers but an ingenious evolutionary tool: the body is going to “yell” louder and louder at you to fix the knee with more and more pain until it gets fixed!
HOW TO FIX KNEE PAIN AND PFPS
I am going to give you every tool I would give to a patient to help themselves with PFPS but there is a catch.
The catch is that stretching, gluteal strengthening, spine care, intrinsic foot exercises and/or orthotics is only going to be effective if the body is working properly. You can read more about the details here but just know that in a huge majority of cases we see, people are already doing the right homework but their body is not working properly. Their efforts are typically not working cause they have a problem with the spine or the nerves that leave it that make the exercises ineffective.
Take my patient ST. ST was having pain with stairs and squats that left her scared and unable to exercise or even move around the house confidently and pain-free. She was doing a lot of the correct exercises to strengthen her hips and glutes but because of a suspected problem with her spine, the gluteal muscles were not activating properly and they were substantially weaker during our NeuroStructural Examination than they should have been for their size. Furthermore, we found that the joint tissues of the affected knee and the obturator, sciatic and femoral nerves that travel towards the knee were substantially more sensitive on the affected side despite it being months since she had a small slip on vacation that started all this!
The solution:
- Correct and restore the proper health of her spine to ensure that the spine and nervous system are not a limiter in the performance of the knee
- Electroacupuncture of the nerves irritated nerves or sensitive tissues around the knee restores a normal Brain-Body Connection and makes them less sensitive
- Restore the activation/Brain-Body Connection of the gluteal muscles so that they can properly control the femur and tracking of the knee and use all of the available muscle mass
- ST did not require arch or ankle support to limit the collapse of her knee because of the foot but it was assessed for
- ST was told to do these exercises daily for the extent of her one-month care plan
Hip strengthening protocol: free HERE
Side Stretch and Gluteus Maximus stretches: free HERE
If you perform these exercises and stretches 2x/day for a month and you do not see a complete resolution of your problem then it is time to get checked for what the underlying problem could be in your case that is causing your knee pain and maybe some other problems you are unaware of!
If you are unsure if moving forward with an examination is right for you that is okay! We always start with a Complimentary Case Review to see if it is a mutually good fit. A consultation is a conversation – not a commitment!
Book here.
Work referenced:
Davis, Irene S., and Christopher Powers, eds. “Patellofemoral pain syndrome: proximal, distal, and local factors—international research retreat, April 30–may 2, 2009, Baltimore, Maryland.” journal of orthopaedic & sports physical therapy 40.3 (2010): A1-A48.