The goal is with any condition is never to just band-aid your pain, but correct the underlying weakness and dysfunctions so that we eliminate the underlying cause and stop the condition from coming back. If you want to know how you can manage or prevent shin splints, also known as medial tibial stress syndrome (MTSS), then check out my condition manual for a more in-depth understanding.
Here is a small excerpt from that article. Understanding the biomechanical changes that lead to a particular condition, is vital in providing the best clinical outcomes and the fastest recovery. Yes, rest will help your symptoms. But simply resting your leg with not stop the underlying cause of the issue, and you are just asking for it to come back. Get your musculoskeletal issues managed properly from someone that understands the underlying causes and how to fix them.
Etiology – What Research Says About Shin Splints
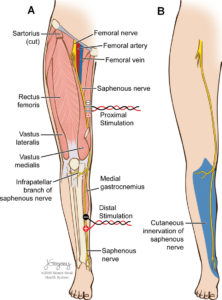
It was once thought that traction from the solueos, tibilias posterior and flexor digitorum longus muscles were implicated in causing this injury through their pull on the bony attachment of the tibia
As tension in these aforementioned muscles increases, the tension in the connective tissue fascia around the muscles and the bones increases proportionally. More tension in the muscles causes more tension and repetitive strain on the bone and its connective tissue layer called the periosteum. As many studies have indicated with diagnostic imaging and evaluation, inflammation and pain generation from the periosteum, called periostitis, seems to be implicated.

The symptoms are however, not always felt at the site of origin of these muscles. Often the pain is located lower on the distal 2/3 of the tibial below where these muscles attach.
Research have worked to explain this discrepancy and have also demonstrated that MTSS is not just pain coming from the periosteal fascial bone tissue but also results from bony changes. MTSS is also a bone injury to the outer cortical bone likely resulting from bending of the tibia.

Imaging studies have shown that there is tibial cortex osteopaenia and, reduced bone mineral density. MRI shows bone marrow oedema (swelling) and periosteal reaction.
When force is put through the tibia at a greater amount or rate than it can adapt to, because of the aforementioned reasons, the bone becomes less dense, more porous and weakens. These bony changes result in pain over time.
MTSS is both a bone and periosteum injury, resulting from a number of causes.
Studies using MRI have shown the MTSS is similar in presentation to a stress fracture but is unlikely to progress to a stress fracture with continued activity. Thus, while MTSS does appear to involve some insult to the bone, I would not recommend complete rest as some would with a fracture. Relative rest from the most insulting activities is likely the best course of action.
My Explanation Of Why We Get MTSS
Every time that your foot strikes the ground, forces enter into the lower limb and have to be absorbed and dissipated. The harder one strikes the ground (running > walking), the more force that enters and must be accommodated. If the ground reaction force entering the foot, ankle, leg, knee and thigh is not properly absorbed by the muscles, other structures like the ligaments, joints, bones, menisci or tendons will. These structures are less adapt and managing the acute forces that come from exercise, and are likely to sustain a repetitive strain injury if they continue to be exposed to the impact about their tolerance threshold.
When it comes to MTSS there are a number of issues, that are supported in the literature, that I see.
Often there is some sort of combination of the following
- increased ankle mobility / flexibility (why orthotics seem to work) causing the ankle to move with greater pronation or collapse that leaves one prone to this condition
- weakness of the leg muscles (gastroc, soleous, fibularus group, deep calf muscles in some combination)
- weaknessoftheglutes (gluteus maximus,minimus and medius) causes relative instability of the hip
- The hip is not strong enough to control how the thigh, knee and leg move when it hits the ground
- Most commonly increased tibial internal rotation or dynamic knee collapse is a consequence of this weakness and likely other muscles attempt to compensate resulting in repetitive strain
- Hypermobility of the lower limb joints exists, often the superior joint between the tibia and fibula, which further increases the challenge of stabilizing the leg
The result is that the calf muscles, ankle and knee are not properly absorbing the force they accepts when the foot hits the ground. An excessive amount of force is delivered into the deep calf muscles, the tibia and the connective covering of the tibia, which results in a repetitive strain injury.There is a lack of stability in the lower limb.
The key is to ensure the joints, muscles, nerves of the leg are working properly so that the impact forces are accepted by the muscles and not being transmitted to the tibia and its periosteum to perpetuate the injury
How We Achieve This
- Rehab exercise therapy to strength the hip musculature and the muscles of the calf to better stabilize the ankle and knee
- Acupuncture (usually electro-acupunture) to help relieve pain at the site of injury and ensure that the nervous system is working properly to control and power the force dampening muscles
- ART or soft tissue massage to balance the tightness of the lower limb muscle, relieve pain at the site of injury and ensure that when they are asked to, the muscles can slide and contract properly to do their job
- (Kinesio)Taping the lower limb can help up to stabilize the joints of the lower limb and redirect force away from the tibia
- Joint mobilizations and manipulations when needed to ensure better joint movement to correct any joint dysfunctions
- Orthotics when applicable and necessary
References
Moen, Maarten H., et al. “Medial tibial stress syndrome.” Sports medicine 39.7 (2009): 523-546.
Michaud, Thomas C. Human locomotion: the conservative management of gait-related disorders. Newton Biomechanics, 2011.